Geographic atrophy (GA) is an advanced form of dry age-related macular degeneration (dAMD) and manifests as a chronic progressive degeneration of the macula that can lead to irreversible vision loss.
References
1. Wong WL, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106-e116.
2. Rudnicka AR, et al. Age and gender variations in age-related macular degeneration prevalence in populations of European ancestry: a meta-analysis. Ophthalmology. 2012;119(3):571-580
3. Friedman DS, et al. Prevalence of age-related macular degeneration in the United States [published correction appears in Arch Ophthalmol. 2011 Sep;129(9):1188]. Arch Ophthalmol. 2004;122(4):564-572.


Complement-only inhibitors have demonstrated promising
efficacy in GA, yet significant treatment burdens exist
Complement (C3 and C5) inhibitors administered by monthly or every-other-month intravitreal injections have efficacy in slowing the progression of GA lesions that is well understood1,2. However, frequent needle injections into the back of the eye is a source of fear, discomfort and disruption for patients3. With current approved complement-only inhibitors, patients may experience 6 to 14 intravitreal needle injections in the eye per year. If patients also have another condition, like choroidal neovascularization that requires treatment with intravitreally-injected VEGF inhibitors, they may experience 12 to 22 injections per year.
References
1. Liao DS, et al., Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration – a randomised phase 2 trial. Opthalmology 2019; 127: 586-195.
2. Jaffe GJ, et al., C5 inhibitor avacincaptad peg for geographic atrophy due to age-related macular degeneration – a randomised pivotal phase 2/3 trial. Ophthalmology 2021; 128: 576-586.
3. McClard CK, et al. Questionnaire to Assess Life Impact of Treatment by Intravitreal Injections (QUALITII): Development of a patient-reported measure to assess treatment burden of repeat intravitreal injections. BMJ Open Ophthalmol. 2021;6(1):e000669.
Choroidal neovascularization (CNV) is a sight-threatening condition that is associated with complement-only inhibitors approved for the treatment of GA
CNV is responsible for 90% of severe vision loss in age-related macular degeneration patients and eyes with CNV experience greater vision loss than GA only. LTB4 can upregulate the production of VEGF-A, a key driver of CNV.3 LTB4 inhibition may prevent choroidal neovascularization.
1
Choroidal neovascularization (CNV) starts with inflammation in the choroid and retinal pigmented epithelium (RPE)
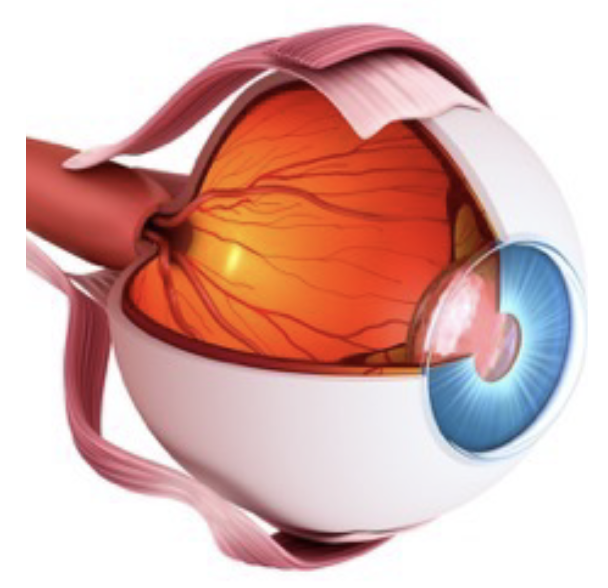
The RPEs ability to cope with stress decreases with age and the subsequent inflammation damages the RPE and photoreceptors2. A damaged RPE releases leukotrienes, including LTB42,3.
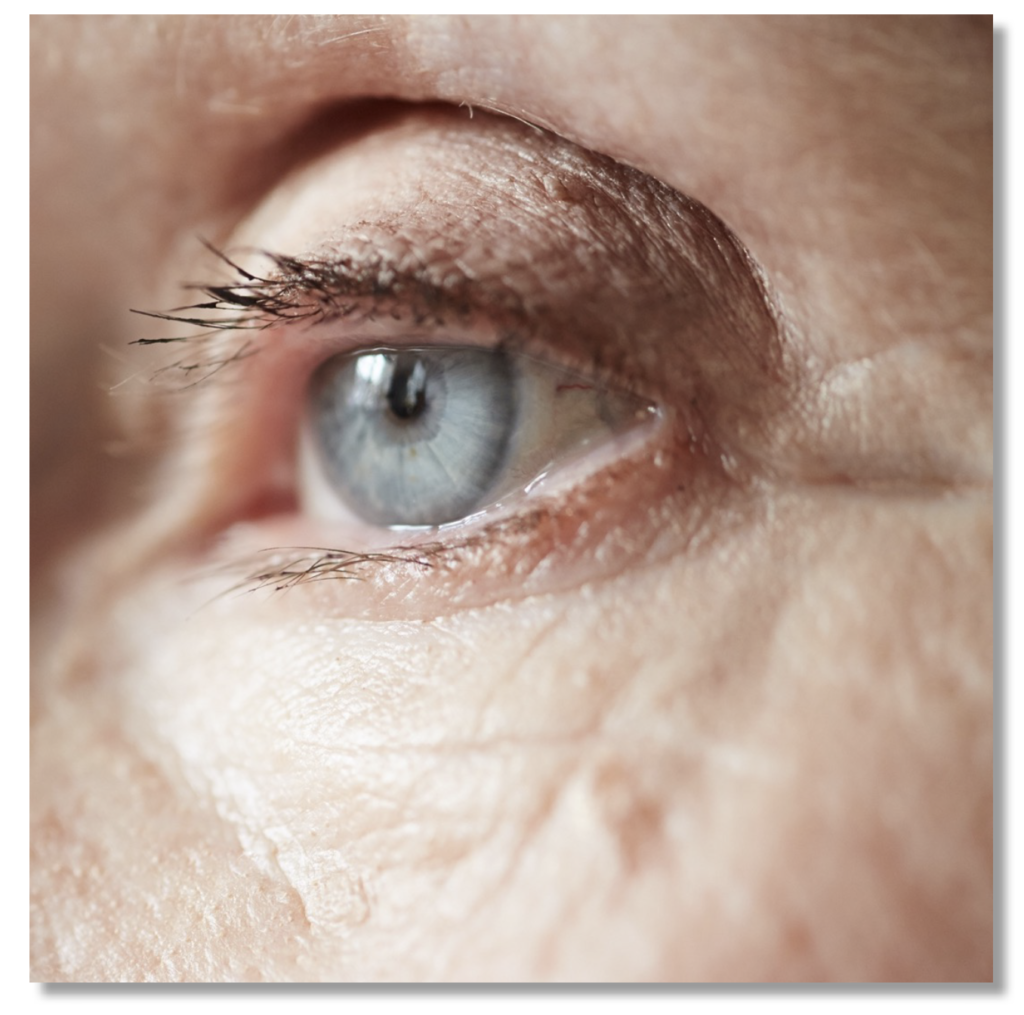
The choroid is part of the vascular layer of the eye1. The RPE, adjacent to the choroid, is constantly exposed to high levels of metabolic and oxidative stress1.
2
LTB4 activation can lead to over expression of VEGF-A

In a pre-clinical model of laser-induced CNV LTB4 recruited inflammatory immune cells into the retina3 M2 macrophages were attracted and activated via LTB4 receptors leading to production of vascular endothelial growth factor–A (VEGF-A)3.
3
Normal expression of VEGF-A is healthy
VEGF-A is one of the key factors responsible for endothelial cell proliferation and migration. Endothelial cells form the inner layer of blood vessels and play a key role in function, including exchanges between blood vessels and surrounding tissues.

4
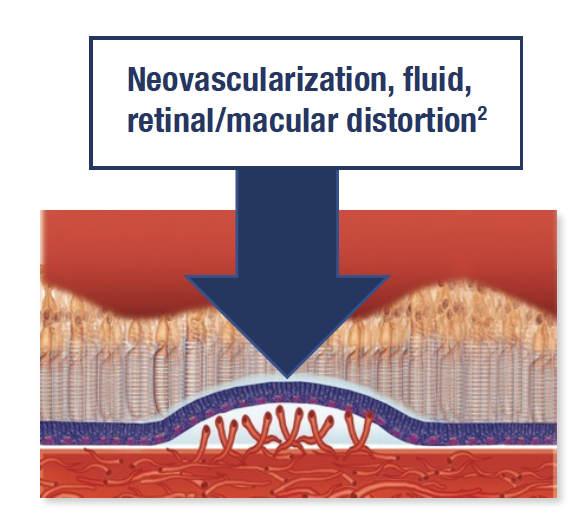
Overexpression of VEGF-A drives choroidal neovascularization
CNV is an overdevelopment of blood vessels in the retina2. New blood vessels are leaky, fluid from blood/ red blood cells enter the retina2. Fluid can distort/damage the retina, including photoreceptors2.
References
1. Hejtmancik JF, Nickerson JM. Overview of the Visual System. Prog Mol Biol Transl Sci. 2015;134:1-4..
2. Grossniklaus HE, Green WR. Choroidal neovascularization. Am J Ophthalmol. 2004;137(3):496-503.
3. Sasaki F, Koga T, Ohba M, et al. Leukotriene B4 promotes neovascularization and macrophage recruitment in murine wet-type AMD models. JCI Insight 2018;3(18):e96902. Published 2018 Sep 20.